25 year old with dengue fever
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box.



Case of a 25 year old female with body ache and fever
This is a case of a 25 year old female, resident of nalgonda who is a homemaker, who presented to OPD 5 days ago with chief complaints of
Generalised body ache since 10 days
Pain in joints of hand and feet since 10 days
Fever since 7 days
History of presenting illness
The patient was apparently asymptomatic 10 days ago when she developed generalised body ache which were sudden in onset, continuous, aggrevating with onset of fever and relieved on taking medication.
10 days ago The patient also developed joint pains first at metacarpophalengeal joints and ankle joints later shoulder joint and knee joint were also involved. The joint pains were dull aching, continuous, did not cause any functional impairment.
7 days ago the patient developed fever which was sudden in onset associated with chills and rigor. No diurnal variation seen. The patient recorded 101-104F fever which relieved temporarily on medication and had no aggrevating factors.
4 days ago the patient consulted local RMP who asked her to get NS1 antigen test, for which she tested positive. After learning the test result, the patient was brought to kims narketpally for treatment.
On the day of admission, the patient developed 4 episodes of vomiting which were non projectile, non blood stained,occured after consumption of food, non bile stained consisting food particles.
Vomiting was not associated with neck rigidity, abdominal pain.
No aggrevating factors noted, relieved spontaneously.
Patient also developed 4 episodes of loose stools which was non blood stained no aggrevating factors, relieved spontaneously after 4 episodes.
No history of giddiness, seizures, blurring of vision.
No history of cough, cold, post nasal drip.
No history of rash.
During admission, Hess test positive
Past history
No similar complaints in past
6 months ago, patient had undergone cesarian section.
Patient is not a known case of diabetes mellitus, hypertension, tuberculosis, asthma, epilepsy.
No history of blood transfusions.
Obstetric history
P1L1
Menarch-13 yrs
Cycles regular 5/30 days
Delivered baby 6 months ago
Lscs
Family history
No similar complaints in the past
Personal history
Appetite- slightly reduced
Diet- mixed
Bowel and bladder movements- regular
Sleep- adequate
Addictions- none
Allergies- none
Community history
The patient travelled to her relatives house 15 days ago, which was surrounded by open fields, stagnant water pools. The patient also mentioned that few of her relative's neighbours were tested dengue postive during the same time.
Daily routine
The patient wakes up at 7 am
Has tea between 8-9am
Consumes breakfast at 9am
Does household chores throughout the day
lunch at 1 PM
Sleeps from 1pm to 4pm
Goes out for walk carrying her new born from 4pm to 6pm
Dinner at 8 pm
Sleeps at 10pm
General Examination
The patient was conscious, coherent and cooperative.
The patient is moderately built and moderately nourished
Vitals:
Blood pressure 110/70 mm hg
Temperature: Afebrile
Pulse rate - 68 beats per minute, normal rhythm, volume ,character, no radio radial or radio femoral delay
Respiratory rate- 22 per minute
Absence of pallor, icterus, cyanosis, clubbing, lymphadenopathy, pedal edema.
Systemic examination
Per_abdomen_
Inspection :
Umbilicus inverted, hernial orifices free, suprapubic transverse scar present, all quadrants move equally with respiration, scaphoid shape.
Palpation :
No local rise of temperature noticed
On superfcial and deep palpation
Tenderness in the right hypochondrium , epigastric region , left hypochondrium and hypogastric region felt by patient.
Percussion
- Tympanic note heard in all 9 segments of the abdomen
Auscultation
- Bowel sounds heard
Cardiovascular system examination :
S1, S2 Heard
No thrills or murmurs
Respiratory system examination
Trachea central in position
Bilateral air entry present
Normal vesicular breath sounds were heard bilaterally in all areas
Central nervous system examination
Higher mental functions normal
No focal neurological deficit found.
Provisional diagnosis: This is a case of a 25-year-old female with body ache associated with joint pains and high-grade fever associated with chills and rigour.
suggestive of dengue
Investigations
NS1 antigen test
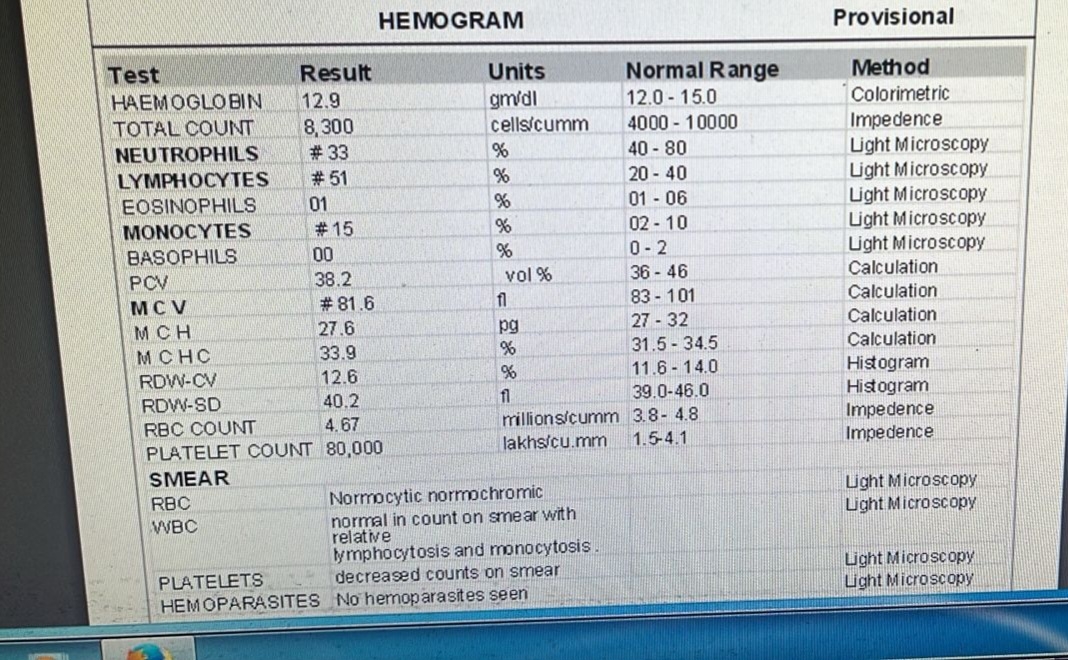
Complete blood picture
Day 1
Day 2
Day 3
Day 4
Electrocardiogram
Ultrasound abdomen
Final diagnosis-
The 25 year old female is suffering with dengue fever.
Treatment
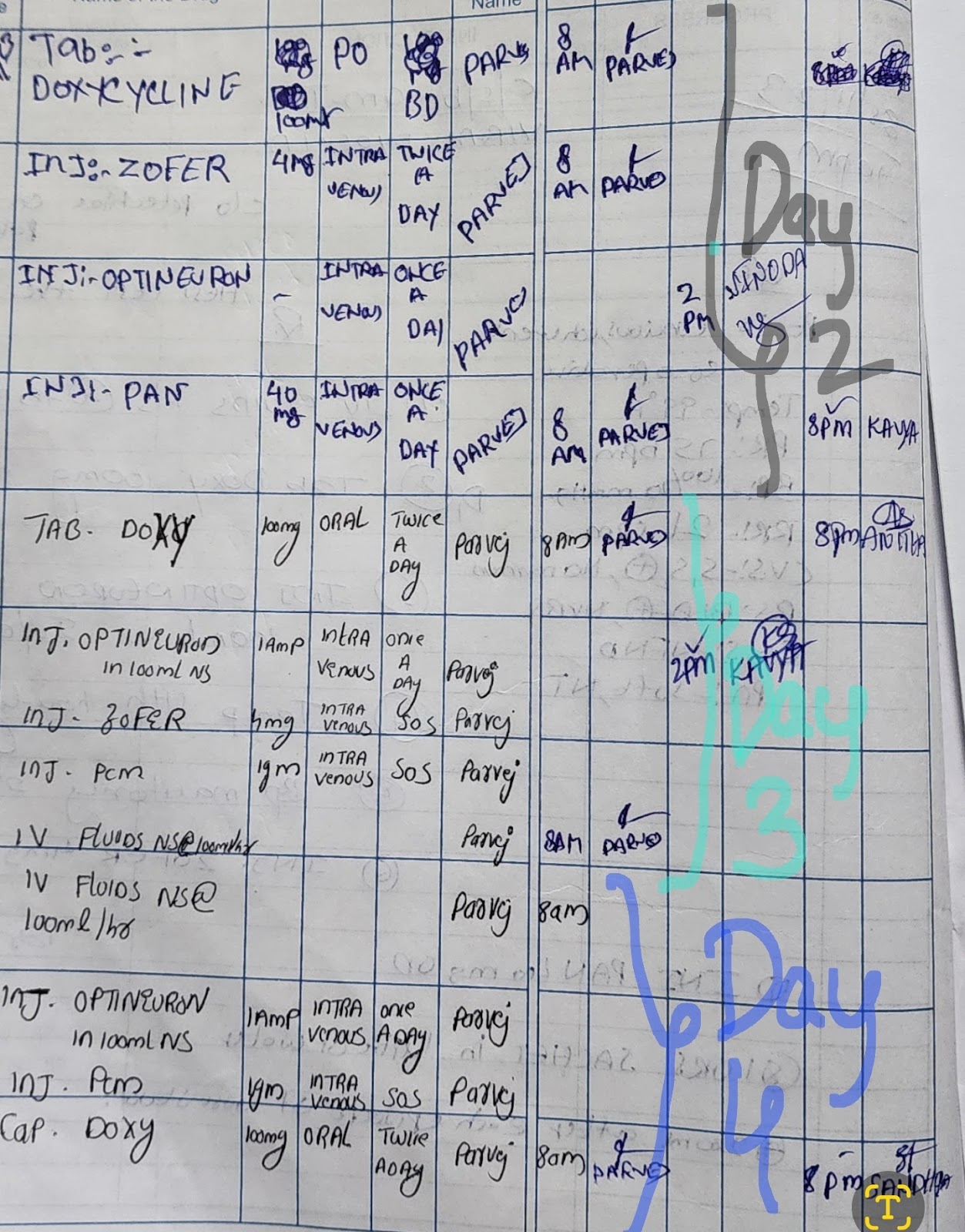
On day-1
IV fluids 75ml/hr
Tab doxycycline 100mg
Inj optineuron
Inj zofer 4mg IV
Inj pan 40
1 ORS sachet
Day 2-4








Comments
Post a Comment