Viswanath Garudadhri
Roll no -147 , 8th sem
Under the guidance of Dr. Niteesh (intern)
This is an online e-log platform to discuss case scenarios of a patient with their guardian's permission.
I have been given this case to solve in an attempt to understand the topic of patient clinical data analysis to develop my competency in reading and comprehending clinical data including, history, clinical findings, investigations, and come up with a diagnosis and treatment plan.
CASE SCENARIO
A 35 yr old male came to OPD with chief complaints of fever, pain in neck, cough, giddiness, lower back pain since 1 week.
HISTORY OF PRESENTING ILLNESS
Patient was apparently asymptomatic 20yrs ago, then started drinking toddy and slowly addicted to whiskey since 2010. One month ago developed blood in stools and itching all over body. Patient experienced episode of loss of consciousness 10 days ago which was sudden. Later developed fever, cough, back pain since 7 days.
After admission into hospital, the patient experienced another episode of loss of consciousness which was 4 days ago.
HISTORY OF PAST ILLNESS
History of alcoholic hepatitis 1 yr back
Not a k/c/o DM, Asthma, Epilepsy, TB, HTN
TREATMENT HISTORY
Baclofen
Supan-40
Lu-zine
PERSONAL HISTORY
Diet - Mixed
Normal appetite
Sleep - Diminished
Bowel and bladder movements - normal
Addictions - has been drinking toddy since 20 yrs.
Has been drinking whiskey since 2010
Last drink - 1/4/2023
No known allergies
History of blood transfusion twice
1st time - 8/4/2023
2nd time - 10/4/2023
FAMILY HISTORY
No data available
GENERAL EXAMINATIONS
Patient is concious, coherent and cooperative
Built - moderate
Nourishment - moderate
Pallor present
No -Icterus/Cyanosis/Clubbing/Lymphadenopathy/Edema/Malnutrition
Temperature -99 F
Pulse rate - 82 /min
Bp - 120/80 mm/hg
RR - 13cycles/min
SpO2 - 98%
SYSTEMIC EXAMINATION
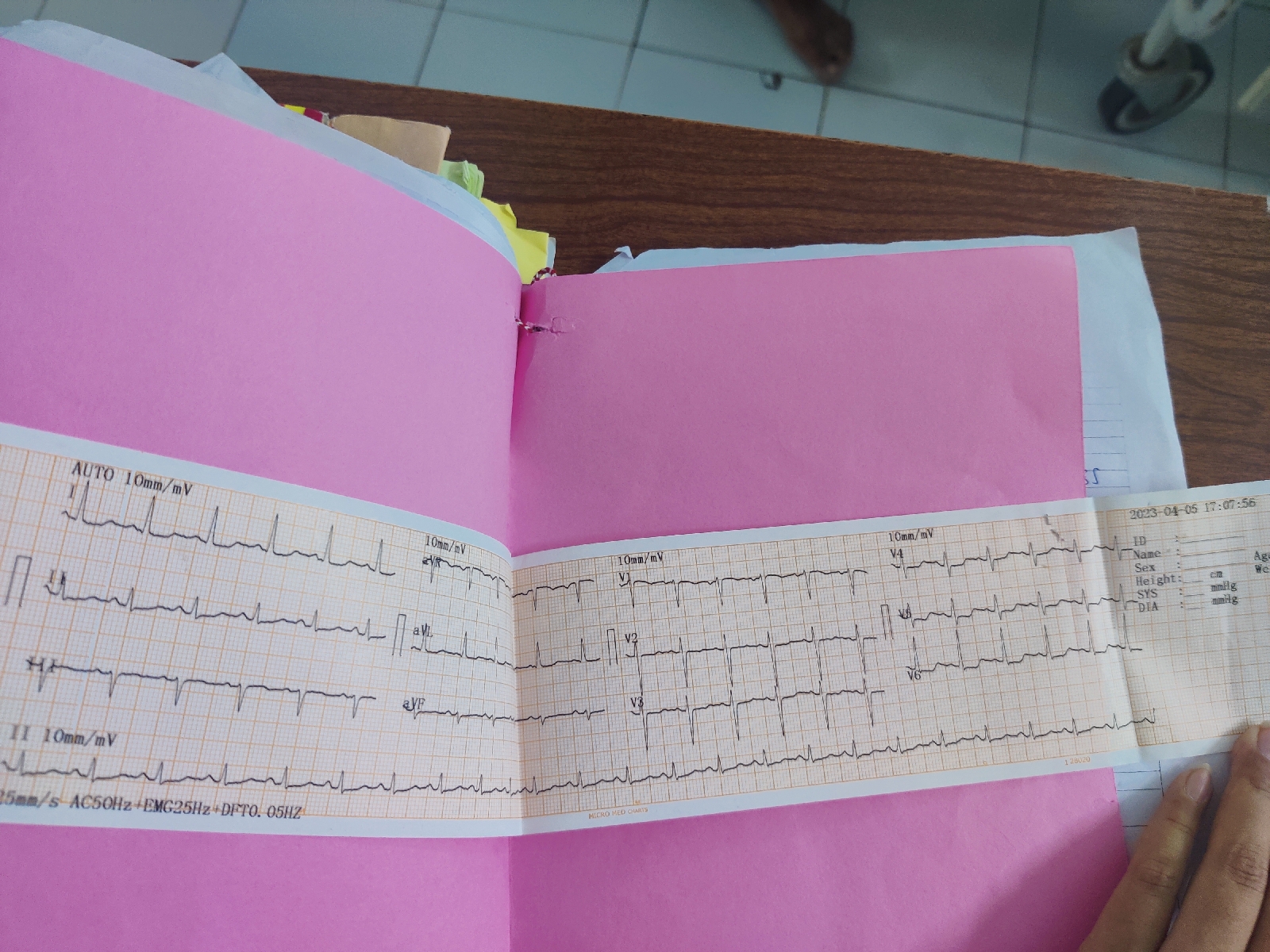
CVS:
No Thrills
Cardiac Sounds - S1, S2 +
No cardiac murmurs
RESPIRATORY SYSTEM:
Dyspnoea - No
No Wheezing
Position of Trachea - central
Vesicular sounds
ABDOMEN:
No palpable mass, No bruits
Liver Spleen - Not palpable
CNS:
Level of consciousness - conscious
Speech - Normal
No signs of meningeal irritation
Cranial nerves - Normal
No motor or sensory deficit
Glassgow scale -15/15
Tab Dolo-650
Tab Lorazepam
Inj Pantaprazole
Inj Ceftriaxone
Inj Frusemide








Comments
Post a Comment